Section menu
Deep Brain Stimulation (DBS) for Tourette syndrome
The available treatments for tics, i.e. behavioural interventions and/or medication, do not always help. In a small number of people with Tourette syndrome (TS), tics can be so severe and extreme that quality of life is significantly impaired, and this often leads to depression, anxiety and isolation. Deep brain stimulation (DBS) has been investigated in adults who are both severely affected by Tourette syndrome and who have not been sufficiently helped by available treatments.
What is DBS?
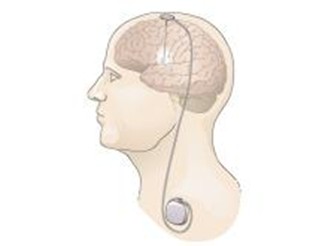
DBS is a neurosurgical procedure during which thin electrodes are introduced into the brain through small holes made in the skull while the person is under anaesthetic. Because the brain is composed of two sides (hemispheres) with the same structures on each side, two electrodes are inserted and the electrode tip placed in the same structure on each side. The top of each electrode is anchored to the skull and attached to a cable which travels under the skin to a battery which is also placed under the skin of the chest (see image).
Thus, the presence of DBS is not obvious externally. The battery delivers a continuous small electrical current to the electrode tips. The amount of electricity being delivered and the precise area of brain being stimulated can be modified by a DBS specialist neurologist or nurse using a device placed over the battery site. The optimal setting is achieved over several hospital visits using feedback from the person with DBS regarding the degree of improvement. If DBS is ineffective, the stimulation can be turned off and the DBS system can be removed.
DBS has been used to treat the abnormal movements seen in Parkinson’s disease for over 25 years. It is performed routinely in specialist neurological centres in UK, and is regarded as a safe and effective procedure. However, there are some neurosurgical complications which can occur around the time of surgery such as a bleed into the brain and infection around the battery site. However, these are uncommon. Since its first use in Parkinson’s disease, DBS has been used to treat other movement disorders such as dystonia and essential tremor.
Does DBS work for Tourette syndrome?
Many research studies have been conducted to assess the effectiveness of DBS. The most stringent research studies are randomised double-blind controlled trials (RCTs). These compare the severity of tics when stimulation is switched on compared to when there is no stimulation being delivered.
The most common measure of severity is the Yale Global Tic Severity Scale (YGTTSS); this is divided into the total tic severity score and an impairment score which reflects how severely tics affect daily life. Importantly, when being assessed, the patients do not know if the DBS is on or off and neither does the person rating the severity of the tics. There have been 6 RCTs to date with relatively few participants, 55 in total. DBS of two different brain structures have been studied – the thalamus and the globus pallidus. Both of these structures are ‘way-stations’ along a brain circuit thought to mediate the initiation and control of movement. This circuit is thought to be dysfunctional in Tourette syndrome. Because of the small number of RCTs so far, ‘meta-analyses’ have been conducted which take account of the data from all RCT studies together.
One rigorous meta-analysis by Wehmeyer and colleagues in 2021 showed a significant reduction in total tic severity score when ‘on’ stimulation was compared to the ‘off’ condition and when DBS of both thalamus and globus pallidus sites were considered together. When each site was considered separately, DBS of the globus pallidus was more effective than the thalamus. The same study also did an analysis which included ‘observational’ studies which reported the effect of DBS compared to pre-DBS. Overall, these studies found a statistically significant reduction in the global YGTSS score, which reflected both tic severity and impairment.
Around two thirds of patients experienced a reduction by at least 50% at 6 months after surgery. Thus, DBS can be very effective in helping control tics and in improving day to day life in people with Tourette syndrome. However, although most experienced some improvement after DBS, a minority had no benefit at all from DBS.
Who can undergo DBS?
DBS is not yet available on the NHS. This is because the evidence is still considered insufficient as few RCTs have been conducted so far. One successful UK RCT has been published to date, and another is underway. However, DBS for Tourette syndrome is offered as a clinical service by some countries if funding is available. DBS for tics is generally restricted to adults when the brain is fully mature, unless a young patient’s life is at risk due to the severity of the tics.
Further Reading
Wehmeyer L, Schüller T, Kiess J, Heiden P, Visser-Vandewalle V, Baldermann JC, Andrade P. Target-Specific Effects of Deep Brain Stimulation for Tourette Syndrome: A Systematic Review and Meta-Analysis. Front Neurol. 2021 Oct 20;12:769275. doi: 10.3389/fneur.2021.769275. eCollection 2021
- This is a rigorous review of the published literature by experts in the field. It provides a systematic review of all published studies at the time (65 studies, 376 patients) and a meta-analysis of the RCTs (6 studies, 55 patients). It concludes that ‘DBS is a clinically effective treatment option for patients with treatment-refractory TS, with all targets showing comparable improvement rates. Future research might focus on personalized and symptom-specific target selection’.
Szejko N, Worbe Y, Hartmann A, Visser-Vandewalle V, Ackermans L, Ganos C, Porta M, Leentjens AFG, Mehrkens JH, Huys D, Baldermann JC, Kuhn J, Karachi C, Delorme C, Foltynie T, Cavanna AE, Cath D, Müller-Vahl K. European clinical guidelines for Tourette syndrome and other tic disorders-version 2.0. Part IV: deep brain stimulation. Eur Child Adolesc Psychiatry. 2022. PMID: 34605960 Free PMC article. Review
- This is a review conducted by European experts which concludes: ‘Although the overall database has increased in size … definite conclusions regarding the efficacy and tolerability of DBS in TS are still open to debate. Therefore, we continue to consider DBS for TS as an experimental treatment that should be used only in carefully selected, severely affected and otherwise treatment-resistant patients.
Kefalopoulou Z, Zrinzo L, Jahanshahi M, Candelario J, Milabo C, Beigi M, Akram H, Hyam J, Clayton J, Kass-Iliyya L, Silverdale M, Evans J, Limousin P, Hariz M, Joyce E, Foltynie T. Bilateral globus pallidus stimulation for severe Tourette's syndrome: a double-blind, randomised crossover trial. Lancet Neurol. 2015 Jun;14(6):595-605. doi: 10.1016/S1474-4422(15)00008-3. Epub 2015 Apr 14.PMID: 25882029.
- This paper describes the UK RCT of DBS of the globus pallidus (GPi). 15 patients were recruited, and 13 patients completed the study. The study concluded that ‘GPi stimulation led to a significant improvement in tic severity, with an overall acceptable safety profile. Future research should concentrate on identifying the most effective target for DBS to control both tics and associated comorbidities and further clarify factors that predict individual patient response’.
This information was produced by Professor Eileen Joyce, Professor of Neuropsychiatry at The Institute of Neurology, University College London, in November 2025.


